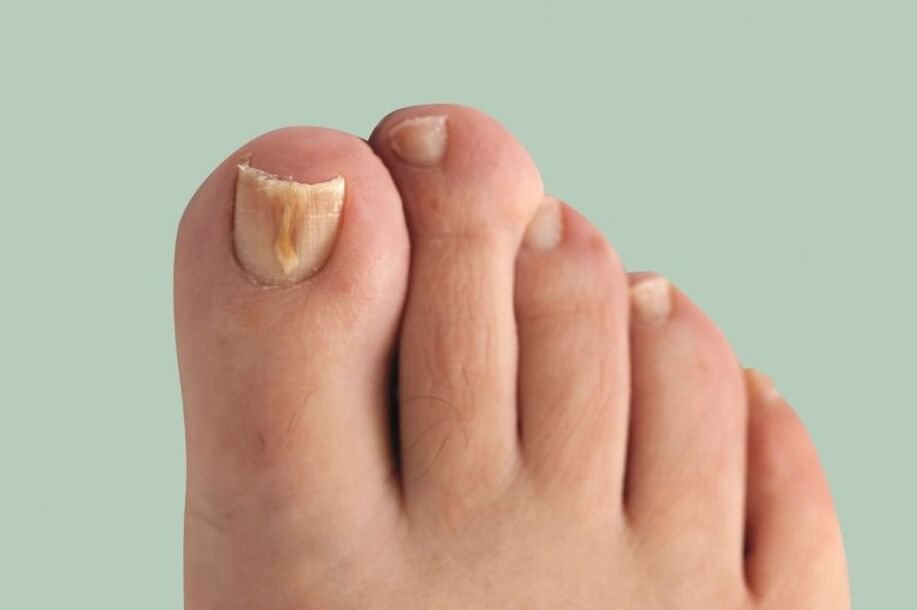
Onychomycosis(nail fungus) is a fungal infection of the nail plate and its surrounding structures: the nail fold, the matrix (the growing part of the nail) and the nail bed. It manifests itself as a deformation and thickening of the nail, a change in color - the nail becomes white or yellow.
This disease is quite common. The prevalence of onychomycosis in Europe, according to some data, reaches 10-12%, exceeding the indicators known in the previous decade. It happens 1. 5 times more often in men, but they go to the doctor 2 times more often than women. Older people get sick more often, children very rarely.
The main problem in treating this disease is that the patient comes to see a dermatologist a long time after the first symptoms appear. Because of this, the pathological fungus covers a wide area and treatment is delayed.
Pathogenic fungi can only be spread by sick people. Often, fungal infections occur in families, because the source is not identified in time and adequate preventive measures are not taken.
Cause of disease:most often in direct contact with the patient or with the objects he uses (shoes, clothes, bath mats, wipes, manicure accessories). Infection often occurs when visiting gyms, baths, saunas and swimming pools.
The development of this disease is facilitated by micro damage - cracks in the interdigital folds that occur due to abrasion, excessive sweating, dry skin, poor drying after water procedures and flat feet.
Nail mycoses can also occur in the presence of concomitant diseases of the endocrine system (diabetes mellitus, obesity, hypothyroidism), vascular diseases of the legs (venous insufficiency, lymphostasis), immune disorders, as well as the use of antibiotics, corticosteroids and cytostatic drugs. As a result of the above diseases, blood microcirculation in the nail area is disturbed and natural immunity is reduced, which contributes to the development of secondary infections.
Onychomycosis is caused by the following types of fungi:
- dermatophytes;
- yeast-like fungi of the genus Candida;
- mold fungus.
Depending on the type of pathogen, the penetration of the fungal infection and the clinical picture occur differently, so the approach to therapy is also different.
Toenails are affected by fungus 10 times more often than fingernails. In most cases, fungus is caused by dermatophytes (for example, Trichophyton rubrum). The remaining cases are most often caused by non-dermatophytic molds (Aspergillus, Scopulariopsis, Fusarium).
If you find similar symptoms, consult your doctor. Do not self-medicate - it is dangerous for your health!
Along with nail fungus, athlete's foot can also develop. Foot mycosis (dermatophytosis, Tinea pedis) is a foot skin disease, caused by pathogenic or opportunistic fungi. Skin changes on the legs are characterized by peeling, which is accompanied by itching. In the case of severe lesions, against the background of red and swollen skin, erosion and deep cracks appear on the soles of the feet and in the space between the toes, which are accompanied by pain and make it difficult to walk.
The advent of modern antifungal drugs has improved the epidemiological situation, but foot mycosis still remains one of the most significant problems in dermatovenerology. The use of some drugs is limited in the elderly and patients with chronic diseases.
Route of infection
The risk of contracting fungus is high especially in public places with high humidity. These are saunas, swimming pools, gyms, public baths, etc. The most common route of infection:
- direct contact with an infected person. Here the fungus moves from its habitat to a healthy area, thereby causing infection;
- household manners. In this case, the infection occurs when using the patient's personal items: shoes, personal hygiene items, etc.
Risk factors
The incidence of onychomycosis increases at the age of 60. Currently, the probability of developing such an infection is 60%, which is explained by the slowdown in metabolism, especially in the distal (distant) parts of the body, i. e. the fingers and toes.
Other risk factors for developing nail fungus include:
- diabetes;
- varicose veins;
- injury to the nail and adjacent tissue;
- HIV and other immunodeficiency conditions;
- long-term use of antibiotics;
- weak immune system;
- vascular and skin diseases, dermatitis, diaper rash;
- disruption in blood supply to the legs;
- inadequate hygiene.
Symptoms of onychomycosis (nail fungus)
The longer the disease lasts, the more pronounced the symptoms. The main symptoms of onychomycosis include:
- dyschromia - a change in nail color to yellow, black, green, gray or brown (the type of color depends on the type of fungus);
- onycholysis - separation of the nail plate from the bed;
- changes in the thickness of the nail plate;
- hapalonychia - a decrease in the thickness of the plate and its softening;
- koilonychia - nails appear concave, in the shape of a teaspoon;
- pachyonychia - thickening of the nail plate, nail hypertrophy;
- onychogryphosis - thickening, discoloration of the nail plate, curved in the form of a beak;
- changes in the thickness of the nail bed (hyperkeratosis - thickening of the nail bed);
- changes on the surface of the nail plate: pits, grooves, ridges;
- changes in the nail folds and surrounding skin (paronychia - inflammation of the proximal nail folds).

It is important to note that none of the symptoms are pathognomonic, that is, uniquely suitable for a particular pathogen, therefore it is impossible to determine them by symptoms - additional examinations are required.
Pathogenesis of onychomycosis (nail fungus)
The pathogenesis of the disease depends on how the fungus gets on the skin and nails.
Distal subungual type:if the fungus has penetrated the skin in the nail fold or distal area, then the infection spreads through the free edge of the nail bed and further into the matrix. At first, the nail plate may not change, but then, due to hyperkeratosis, it gradually moves away from the nail bed and becomes yellowish. The nail plate may gradually thicken.
Surface white type:If a whitish lesion forms on the surface of the nail, then over time the fungus takes over the entire nail plate. The nail thickens, crumbles, and acquires a gray-brown color. In this case, the matrix and epithelium of the nail bed are not affected. No inflammation of the surrounding skin.
Proximal subungual type:the fungus can spread from the skin and periungual folds to the nail plate and then to the matrix, reaching the distal part of the nail plate. Spots appear on the nail in the area of the hole and nail bed, and detachment of the nail plate occurs. There was no significant inflammation of the nail bed or matrix.
Total dystrophic type:The entire nail is affected. The proximal part of the nail fold disappears or thickens until the nail plate can no longer form or grow.
existsbiophysical concept of onychomycosis pathogenesis, who stated that during disease there is a confrontation between two forces: the fungal colony growing towards the matrix, and the natural growth of the nail from the matrix to the distal edge. Therefore, the speed of nail growth is important during onychomycosis - the faster the nail grows, the faster healing will occur. Perhaps this is what explains the low prevalence of this disease in children, because their nails grow faster than adults and the elderly.
Classification and stages of development of onychomycosis (nail fungus)
There are the following classifications of oncomycosis:
- distal subungual;
- shallow white;
- proximal subungual;
- total dystrophic.

According to Arievich's classification (1970):
- normotrophic: in the thickness of the nail there are bands of yellowish and whitish color, but the shape of the nail plate does not change, there is no subungual hyperkeratosis;
- hypertrophic:the nail plate turns yellow, thickens due to subungual hyperkeratosis, becomes brittle, with jagged edges;
- dystrophic:thinning and detachment of the nail plate from the nail bed occurs with the formation of voids.
Complications of onychomycosis (nail fungus)
Long-term onychomycosis increases the risk of developingdiabetic foot(formation of trophic ulcers on the legs) andgangreneif the patient has diabetes mellitus or vascular disease in the lower leg.

In immunosuppressive conditions (primary and secondary immunodeficiencies), fungi can spread to the skin, internal organs and cause body allergies. This can manifest itself as a skin rash and even the development of bronchial asthma.
In an uncomplicated course, the disease causes traditional symptoms for fungi, causing only severe discomfort to a person. But without treatment, onychomycosis can cause complications. Often they manifest themselves in the addition of bacterial infections.
Sometimes onychomycosis is very acute with the appearance of blisters, ulcers and weeping areas on the skin next to the nail. In severe cases, the disease takes a generalized form. This means that the nail fungus spreads to internal organs and systems, and then the patient will need emergency hospitalization.
Diagnosis of onychomycosis (nail fungus)
Before studying the methods for diagnosing onychomycosis, it is necessary to explain how to properly collect material for research (patients do this independently, or prepare nails before diagnosis). Before collecting material for research, it is necessary to treat the nail plate with 70% alcohol to avoid contamination with other bacteria.
The method of collecting material varies depending on the form of onychomycosis:
- surface shape- make a scraping from the nail plate;
- distal form- both scraping from the nail bed and a piece of the nail plate is necessary;
- proximal subungual shape- material is collected with a drill, or a nail biopsy is performed, or a scraping from the nail bed is performed.
The fastest method to determine the pathological fungus in the nail ismicroscope. Technique: the studied material is treated with an alkaline solution to dissolve the keratin. To make the mushroom thread more visible, ink is added to the alkali. Next, the resulting preparation is studied under a microscope.
This research method is the fastest and most objective. Sensitivity is up to 80%. The disadvantages of the method include the fact that when using it it is impossible to determine the type of pathogen.
Bacteriological culture: is an additional method to diagnose onychomycosis. The material is seeded on a special medium and the results are interpreted under a microscope after 2-3 weeks. This method allows you to determine the type of pathogen - this helps in determining treatment tactics and in choosing drugs based on sensitivity. But the disadvantage of the study is that it takes a lot of time, and the sensitivity is only 30-50%.
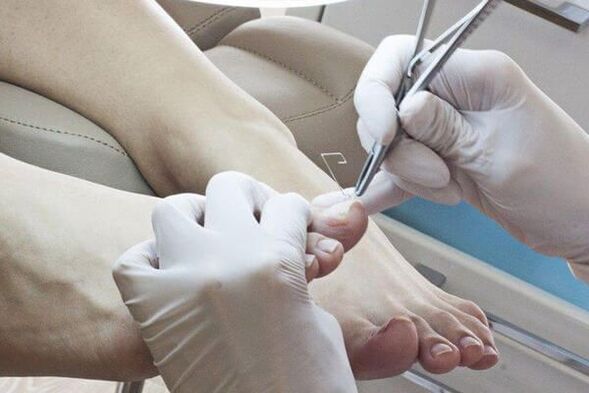
Biopsy: Using a scalpel and using anesthesia, nails and nail beds are cut. The material is soaked in formaldehyde solution and sent for histological examination to the laboratory. The advantage of this method is that it is very sensitive and allows you to determine the presence of pathological fungi in the material.
Disadvantages: it is impossible to identify pathogens, as well as establish the viability of microorganisms, the method is expensive and labor intensive.
Gene diagnostics: molecular biology research method (PCR). This is one of the new and very sensitive methods for diagnosing onychomycosis - it helps to detect the DNA of the causative agent of this disease. In our country, it is recommended to introduce this type of diagnostics in medical institutions that have a PCR laboratory, but at the moment, the test system to identify dermatophytes and molds is only planned to be introduced into the laboratory. This method allows you to determine the type of pathogen, and the sensitivity ranges from 80-90%. Disadvantages: high cost, inaccessibility, lack of technological standards and complexity of implementation.
More and more, doctors introduce into practicedermatoscopy. Using this method, you can evaluate changes in the color and structure of the nail, as well as the condition of the surrounding structure. Dermatoscopic examination allows a more accurate assessment of the depth of damage to the nail plate and a more correct calculation of the severity index of onychomycosis (KIOTOS).
First of all, the patient is sent for a microscope, which allows to identify the presence of pathogens. In the future, it is necessary to determine the type in order to choose the right treatment for toenail fungus. At JSC "Medicine" (academic Roitberg's clinic) in the center of Moscow, the most modern and widespread methods of diagnosing onychomycosis are practiced:
- cultural examination of biological samples of affected tissues. To do this, it is placed in an artificial nutrient medium, where the pathogen is grown to determine its type;
- polymerase chain reaction (PCR) method to detect pathogen DNA in affected tissue samples.
When you see a doctor
Many who have experienced onychomycosis know that this disease develops slowly and is very difficult to treat. That is why it is very important to consult a doctor when the first signs of the disease appear. Dermatologists treat nail onychomycosis in our clinic in the center of Moscow. Specialists will provide efficient assistance and will guide you until complete recovery.
Prepare to visit the doctor
Before visiting a dermatologist, it is important not to treat the affected nail area with anything, i. e. do not use medicines, including iodine and brilliant green. It is also necessary to avoid the use of creams and ointments against fungus. At your appointment, you will need to take all the tests taken before, including tests for other diseases. The affected nail should not be cut for 3-4 days before the consultation.
Treatment of onychomycosis (nail fungus)
There are several types of treatment for onychomycosis:
- Local therapy.
- Systemic therapy.
- Combination therapy.
- Corrective therapy.
Local therapyinvolves the use of medication on the nail plate and nail folds. Indications for local therapy:
- A limited form of damage to the nail plate (according to KIOTOS).
- There are contraindications to prescribing systemic drugs: hypersensitivity, liver disease, kidney dysfunction, pregnancy, breastfeeding.
The advantage of this therapy is that a high concentration of the therapeutic agent is formed on the surface of the nail, which does not penetrate the bloodstream. There are no side effects of using antifungal drugs - nausea, loss of appetite, stomach pain. The disadvantage of this method is that the medicinal substance does not always reach the habitat of the pathogen, especially if the fungus is located at the base of the nail or the matrix. This in turn can lead to treatment failure. This type of treatment is very labor intensive, because before using the medicine it is necessary to remove the affected part of the nail.
Methods for removing affected nails:
- Mechanical removal using files, clamps or drills.
- Using a keratolytic patch. Before applying the keratolytic plaster, the skin around the nail is covered with a plaster, a plaster mass (urea with salicylic acid) is applied on top and sealed with an adhesive plaster. The plaster mass is changed every 2-3 days. After each removal, the affected part of the nail is removed mechanically.
- Surgery. This operation is very painful and traumatic, because when the nail plate is removed, the growth zone can be damaged, which leads to the regrowth of the deformed nail.
Local antifungal agents are used after removing the affected nail plate.Antimycoticsdifferentiated according to the place of application:
- used on nails: varnish;
- used for rollers: creams, ointments, solutions.
The most studied drug for topical use is1% naftifine solution, which has an evidence base for efficacy in treatment based on a Cochrane meta-analysis. The product is water-based, which facilitates better penetration of the antifungal agent into the affected area. Varnish, the active ingredients of which are ciclopirox and amorolfine, have a dehydrated base, which reduces the penetration of the drug into the inner layer. Therefore, dermatologists consider the use of varnish unsatisfactory and increasingly choose water-based products.
To get results from local therapy, it is necessary to follow the treatment regimen; it is important for patients to be responsible, consistent and patient. The duration of therapy can be up to 12 months.
Systemic therapyallows the antifungal drug to penetrate the bloodstream to the site of the lesion, even if the nail bed and matrix are affected. A high concentration of the drug remains in the affected area for a long time after the end of use. The disadvantage of this type of treatment is associated with the risk of side effects and toxicity.
Indications for systemic therapy:
- A common form of nail plate damage.
- Less effective than local therapy (ie, after six months of treatment for onychomycosis on the hands and 9-12 months of treatment for onychomycosis of the feet, healthy nails do not grow back).
To determine treatment tactics, KIOTOS (Clinical Index for Assessing the Severity of Onychomycosis by Sergeev), proposed by A. Yu. Sergeev in 1999, used. It is used as a therapeutic standard in various countries around the world.
Medicinesfor the treatment of onychomycosis can be classified as follows:
- antimycotic - has an antifungal effect;
- antiseptic - has both antifungal and antibacterial effects. They are rarely used, only in the absence of other antifungal agents;
- multicomponent - in addition to antifungal agents, they also contain other drugs, such as anti-inflammatory drugs.
Prescription regimen:
- standard - take the medicine every day during the prescribed treatment period;
- shortened - the duration of treatment is shortened, can be carried out in the usual dose or increased;
- intermittent - treatment is prescribed in several short courses, the interval between courses is equal to the duration of the course;
- pulse therapy - treatment is prescribed in several short courses, the interval between courses is longer than the duration of the course.
Antifungal drugs are divided according to active ingredients:
- triazole;
- allylamines;
- other (third generation drugs).
Currently used for systemic therapyonly third generation drugs.
With combination therapylocal and systemic treatment is carried out simultaneously. Combination therapy is used when necessary to increase the effectiveness of systemic therapy and reduce treatment time.
Corrective therapy(treatment of concomitant diseases): to choose a treatment regimen, it is necessary to assess the general somatic condition of the body. Diseases such as circulatory disorders in the legs can reduce the access of antifungal agents to the lesions. Therefore, drugs are prescribed that increase tissue trophism.
Due to the toxic effects of systemic antifungal drugs, it is necessary to exclude liver disease and, if necessary, prescribe hepatoprotectors.
Home treatment
Before using home remedies, you should consult your doctor. With his permission, you can use the following recipe:
- iodine. Before use, the feet must be steamed, washed with laundry soap, and then the affected area of the nail plate must be removed. Next, treat the nails and the skin between the fingers with iodine, soak in a bath with soda solution for 20-30 minutes and dry thoroughly;
- vinegar. For 3 liters of water take 1 tablespoon. apple cider vinegar and add a little potassium permanganate. Soak your feet in the bathtub for 20-30 minutes, then dry them thoroughly;
- hydrogen peroxide. After steaming your feet thoroughly, remove the affected area of the nail plate. Put a cotton pad soaked in hydrogen peroxide on them, wrap it with a bandage and leave it for half an hour.
Myths and dangerous misconceptions in the treatment of nail fungus
One of the most important and dangerous myths is that nail fungus is not considered a serious disease. In fact, onychomycosis, as it develops, can lead to serious consequences, including deformation and complete rejection of the nail from the nail bed.
In addition, the infected person poses a daily danger to his loved ones, since being close to him, they are also at risk of getting sick. That is why it is important to know how to cure nail fungus in time.
Prediction. Prevention
The sooner the patient consults a doctor with signs of fungal nail infection, the sooner the disease can be cured and the nail plate restored. With a long-term process involving the entire nail, the treatment of onychomycosis can be long, but if all recommendations are followed, recovery often occurs. If there are contraindications to systemic therapy, long-term maintenance treatment with local drugs is necessary.

For preventionIt is necessary to observe the rules of personal hygiene and reduce the possibility of re-infection:
- try to wear comfortable and high-quality shoes (to avoid excessive sweat on the feet);
- It is recommended to change socks and tights every day;
- use individual shoes only. For those undergoing treatment for onychomycosis, shoes must be treated at the beginning of treatment, at least once a month during the treatment period and after completion;
- if necessary, use an antiperspirant for the feet;
- use an individual nail care kit (scissors, file);
- before and after visiting public places (swimming pools, bathhouses, gymnasiums) use antifungal external agents (sprays, creams and pencils);
- identify the cause of the fungal infection in the family and treat it at the same time.
It is recommended to periodically carry out antifungal treatment of personal items, shoes, bathtubs, floors and carpets. For this purpose, you can use a 40% acetic acid solution, a 1% alcohol solution of chlorhexidine (prescribed by a doctor), and a disinfectant solution. Linen can be boiled in a 1-2% soap-soda solution for 20-30 minutes, ironed at maximum temperature.























